In the realm of reproductive health, the HSG (hysterosalpingography) test plays a pivotal role in evaluating the fertility status of women. This X-ray procedure provides invaluable insights into the condition of the uterus and fallopian tubes, aiding in the identification of potential obstacles to conception and guiding subsequent treatment decisions.
Explanation of HSG Test
The HSG test is a diagnostic procedure utilized to visualize the interior of the uterus and fallopian tubes. Through the use of X-ray imaging, a contrast fluid is introduced into the reproductive organs, allowing for clear visualization of their structure and function. By examining the images produced during the procedure, healthcare providers can detect any abnormalities or blockages that may impede the natural process of conception.
Purpose of the Test
The primary objective of the HSG test is to assess the patency of the fallopian tubes and the condition of the uterine cavity. These aspects are crucial for successful natural conception, as any obstruction or irregularity within the reproductive tract can hinder the fertilization process. By evaluating the integrity of the fallopian tubes and the uterine environment, healthcare providers can determine the likelihood of achieving pregnancy without intervention.
Procedure Details
During the HSG test, the patient lies on an examination table while a specialized X-ray machine is positioned above the pelvic region. A thin catheter is inserted through the cervix into the uterine cavity, allowing for the controlled administration of the contrast fluid. As the contrast fluid fills the uterus and flows through the fallopian tubes, X-ray images are captured in real-time, providing detailed visualization of the reproductive anatomy. The entire procedure typically takes around 15 to 30 minutes to complete and is performed in a clinic or hospital setting under the supervision of trained medical personnel.
Timing of the Test
Ideally, the HSG test is scheduled after menstruation and before ovulation to ensure the patient is not pregnant. This timing helps minimize the risk of exposing a developing embryo to radiation during the procedure. By conducting the test during this window in the menstrual cycle, healthcare providers can obtain accurate results while ensuring the safety of the patient.
Potential Side Effects
Like any medical procedure, the HSG test carries the risk of potential side effects, although they are generally mild and transient. Common side effects may include temporary discomfort or cramping during the procedure, which typically subsides shortly afterward. Some women may also experience light spotting or vaginal discharge following the test. While rare, more serious complications such as pelvic infection or allergic reactions to the contrast fluid can occur. It is essential for patients to discuss any concerns or unusual symptoms with their healthcare provider promptly.
Cost Considerations
The cost of an HSG test can vary depending on various factors, including geographic location, healthcare provider, and insurance coverage. In some cases, the test may be covered partially or fully by insurance plans, reducing out-of-pocket expenses for the patient. However, individuals should verify coverage with their insurance provider beforehand and inquire about any associated co-pays or deductibles. For those without insurance or facing financial constraints, some healthcare facilities may offer payment plans or financial assistance programs to help offset the cost of the procedure.
Interpreting Results
Upon completion of the HSG test, the resulting images are carefully analyzed by radiologists or fertility specialists to assess the condition of the reproductive organs. Clear and unobstructed fallopian tubes are indicative of normal tubal patency, suggesting favorable conditions for natural conception. Conversely, the presence of blockages, abnormalities, or irregularities within the fallopian tubes or uterine cavity may indicate underlying fertility issues that require further evaluation and treatment. Depending on the findings, additional diagnostic tests or fertility treatments may be recommended to address any identified concerns and optimize the chances of achieving pregnancy.
Follow-Up Actions
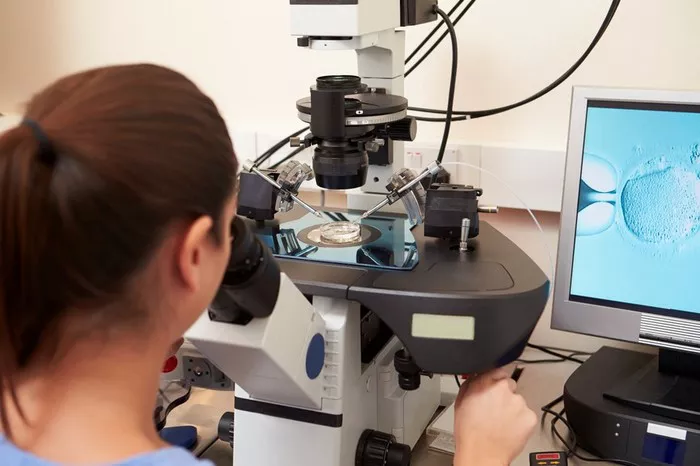
In the event that the HSG test reveals abnormalities or impediments to fertility, healthcare providers will outline appropriate next steps to address the underlying issues. This may involve further diagnostic procedures, such as laparoscopy or hysteroscopy, to provide a more detailed assessment of the reproductive anatomy. Additionally, fertility treatments such as intrauterine insemination (IUI) or in vitro fertilization (IVF) may be recommended to overcome specific challenges and facilitate conception. By proactively addressing any identified fertility issues, individuals can work towards achieving their reproductive goals with the guidance and support of their healthcare team.
Conclusion
The HSG test serves as a valuable tool in the evaluation of female fertility, providing crucial information about the condition of the uterus and fallopian tubes. By undergoing this diagnostic procedure, women can gain valuable insights into their reproductive health and take proactive steps towards addressing any identified concerns. With proper timing, interpretation, and follow-up care, the HSG test empowers individuals to make informed decisions about their fertility journey and pursue appropriate interventions as needed.