Female infertility remains a significant concern worldwide, impacting millions of individuals and couples. According to the latest data, approximately 10-15% of couples globally experience infertility, with female factors contributing to about 40-50% of these cases. These statistics underscore the widespread nature of the issue and the need for comprehensive research and support services.
Trends Over Time
Over the years, there has been a noticeable increase in the prevalence of female infertility, attributed to various factors such as delayed childbearing, lifestyle changes, environmental pollutants, and underlying health conditions. While exact figures vary, the trend suggests a steady rise in infertility rates, prompting greater attention from healthcare professionals and policymakers.
Regional Differences
Regional variations in infertility rates are evident, with some areas reporting higher prevalence rates than others. Factors such as socioeconomic status, access to healthcare, cultural norms, and environmental factors contribute to these disparities. For instance, developed countries typically have higher rates of infertility due to delayed childbearing and lifestyle factors, while developing regions may face challenges related to inadequate healthcare infrastructure and limited access to fertility treatments.
Age-Related Data
Age is a critical determinant of female fertility, with fertility declining significantly after the age of 35. Women in their late 30s and 40s often experience decreased ovarian reserve and increased risk of chromosomal abnormalities, leading to higher rates of infertility and pregnancy complications. Understanding the age-specific infertility rates is crucial for informed family planning and fertility preservation decisions.
Causes and Risk Factors
Several factors contribute to female infertility, including ovulatory disorders, tubal blockages, uterine abnormalities, endometriosis, and genetic factors. Lifestyle factors such as smoking, excessive alcohol consumption, obesity, and stress can also impact fertility. Additionally, certain medical treatments, such as chemotherapy and radiation therapy, can affect ovarian function and fertility potential.
Impact of Infertility
Infertility can have profound psychological, social, and economic impacts on individuals and couples. The emotional toll of infertility often leads to feelings of sadness, stress, and inadequacy, straining relationships and affecting mental well-being. Social stigma and societal pressure further exacerbate the emotional burden, while the financial costs associated with fertility treatments can pose significant challenges for many couples.
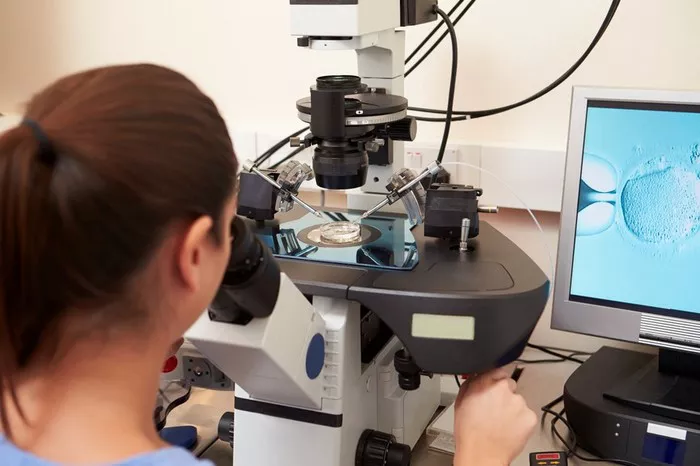
Treatment and Access
Advancements in assisted reproductive technologies (ART), such as in vitro fertilization (IVF), have revolutionized infertility treatment, offering hope to millions of couples worldwide. However, access to these treatments remains unequal, with disparities existing across regions and socioeconomic groups. Limited insurance coverage and high out-of-pocket expenses pose barriers to access, highlighting the need for greater affordability and equity in healthcare services.
Preventive Measures
While not all causes of infertility are preventable, adopting a healthy lifestyle can optimize fertility potential and reduce the risk of certain underlying conditions. Maintaining a balanced diet, engaging in regular exercise, avoiding smoking and excessive alcohol consumption, managing stress, and practicing safe sex can promote reproductive health and overall well-being.
Policy and Healthcare Systems
The role of policy and healthcare systems in addressing infertility cannot be overstated. Comprehensive reproductive health policies, public financing initiatives, and insurance coverage for fertility treatments are essential for ensuring equitable access to care. Investing in infertility research, education, and awareness campaigns can also help destigmatize infertility and promote early intervention and support services.
Future Projections
Looking ahead, infertility rates are expected to continue rising, driven by demographic shifts, lifestyle factors, and environmental influences. However, advancements in reproductive medicine, such as artificial gametes, gene editing technologies, and personalized treatments, hold promise for improving fertility outcomes and expanding treatment options. Collaborative efforts from policymakers, healthcare providers, researchers, and advocacy groups will be crucial in addressing the evolving challenges of female infertility in the years to come.
Conclusion
In conclusion, understanding female infertility statistics in 2024 requires a comprehensive examination of global trends, regional variations, age-specific data, causes, impacts, treatments, preventive measures, policy implications, and future projections. By addressing these key aspects, stakeholders can work towards improving fertility outcomes and supporting individuals and couples affected by infertility.