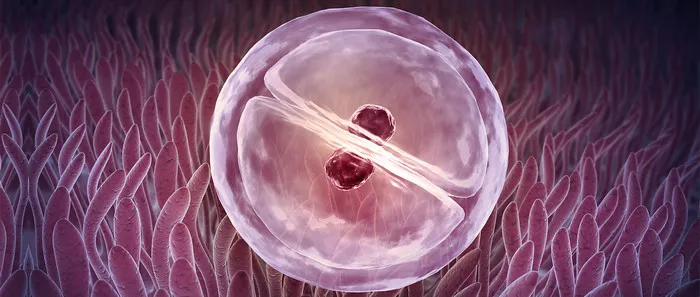
Miscarriage, the loss of a pregnancy before 20 weeks, is a heartbreaking event for any couple trying to conceive. In natural pregnancies, miscarriage occurs in about 10-20% of recognized pregnancies. However, when it comes to pregnancies conceived through In Vitro Fertilization (IVF), the risk of miscarriage may vary. Understanding the factors influencing miscarriage rates in IVF pregnancies is crucial for couples undergoing fertility treatments.
Age and Miscarriage Rates
Maternal age plays a significant role in miscarriage rates, both in natural and IVF pregnancies. As women age, the risk of miscarriage increases. In natural pregnancies, this risk starts to rise around the age of 35 and accelerates after 40. Similarly, in IVF pregnancies, advanced maternal age is associated with higher miscarriage rates. This emphasizes the importance of timely fertility interventions for women in their late 30s and 40s to mitigate the risk of miscarriage.
Thyroid Stimulating Hormone (TSH) Levels
Thyroid health is crucial for a successful pregnancy, whether conceived naturally or through IVF. Abnormal thyroid function, especially elevated TSH levels, has been linked to an increased risk of miscarriage. Therefore, it’s essential to assess thyroid function before undergoing IVF treatment. If TSH levels are abnormal, appropriate medication should be initiated at least a month before egg retrieval to optimize thyroid function and reduce the risk of miscarriage.
Hysteroscopy
Before embarking on the IVF journey, couples should consider a hysteroscopy. This minimally invasive procedure allows for the visualization of the uterine cavity, helping to identify and treat any abnormalities that may contribute to miscarriage. Uterine anomalies such as fibroids, polyps, or septums can impact implantation and increase the risk of miscarriage. Addressing these issues before IVF can improve the chances of a successful pregnancy.
Progesterone Support
Progesterone plays a crucial role in maintaining pregnancy by supporting the uterine lining and preventing early pregnancy loss. In IVF cycles, supplemental progesterone is often prescribed to support implantation and early pregnancy. Various forms of progesterone supplementation are available, including vaginal suppositories and intramuscular injections. Recent studies have shown comparable efficacy between these forms, but individual patient preferences and tolerability should be considered when choosing the appropriate regimen.
Healthy Lifestyle
A healthy lifestyle is essential for optimizing fertility outcomes, especially during IVF treatment. Both partners should aim to adopt healthy habits at least three months before starting IVF. This includes quitting smoking and limiting alcohol consumption, as these habits can adversely affect sperm and egg quality. Moderate exercise and maintaining a normal BMI are also important components of a healthy lifestyle that can positively impact IVF success rates.
Diet
Nutrition plays a critical role in fertility and pregnancy outcomes. While there is no one-size-fits-all diet for IVF success, following a balanced diet, such as the Mediterranean diet, may improve outcomes for non-obese women undergoing fertility treatment. The Mediterranean diet, rich in fruits, vegetables, whole grains, and healthy fats, has been associated with improved fertility and lower miscarriage rates. However, individual dietary preferences and needs should be taken into account when planning meals during IVF treatment.
Coping with Loss
Experiencing a miscarriage after IVF can be emotionally devastating for couples. It’s essential to acknowledge and process the grief associated with pregnancy loss before considering another fertility cycle. Seeking support from loved ones, counseling, or support groups specializing in infertility can help couples navigate the emotional challenges of miscarriage and find healing. Taking the time to grieve and heal emotionally is essential before embarking on another fertility journey.
Chromosomal Testing
Preimplantation genetic diagnosis (PGD) offers couples undergoing IVF the option to screen embryos for chromosomal abnormalities before implantation. By selecting chromosomally normal embryos for transfer, the risk of miscarriage due to chromosomal abnormalities is significantly reduced. PGD may be particularly beneficial for couples with a history of recurrent miscarriage or advanced maternal age, providing them with greater confidence in the viability of their embryos.
Monitoring for Infections
Infections can pose a risk to pregnancy and increase the likelihood of miscarriage. It’s essential for couples undergoing IVF to take precautions to avoid infections and maintain good vaginal health. Practicing safe sex, avoiding exposure to sexually transmitted infections, and following proper hygiene practices can help reduce the risk of infections during IVF treatment. Regular monitoring of vaginal and cervical health during pregnancy is also important for early detection and treatment of any infections that may arise.
Regular Medical Check-ups
Regular medical check-ups are crucial throughout the IVF process to monitor the health of the pregnancy and adjust treatments as necessary. Close monitoring allows healthcare providers to detect any issues early and intervene promptly to optimize pregnancy outcomes. During pregnancy, regular prenatal visits enable healthcare providers to assess fetal growth and development, monitor maternal health, and address any concerns or complications that may arise. Open communication between patients and healthcare providers is key to ensuring the best possible outcomes for IVF pregnancies.
Conclusion
In conclusion, while miscarriage is a risk associated with IVF pregnancies, there are steps that couples can take to minimize this risk and optimize their chances of a successful pregnancy. By addressing factors such as age, thyroid health, uterine abnormalities, progesterone support, lifestyle factors, diet, emotional well-being, chromosomal testing, infection prevention, and regular medical monitoring, couples can enhance their chances of achieving a healthy pregnancy after IVF. Through careful planning, proactive management, and ongoing support, couples undergoing IVF can navigate the challenges of fertility treatment and move closer to realizing their dream of parenthood.
Related Topics:
The Fallopian Tube Damage: Everything You Need To Know
Top Countries for IVF Success Rates: What You Need to Know
The Link Between Epididymitis and Infertility: A Complete Overview