In Vitro Fertilization (IVF) stands as a beacon of hope for countless individuals and couples facing the challenging journey of infertility. It’s a revolutionary assisted reproductive technology that has transformed the landscape of fertility treatment worldwide. Understanding the intricacies of IVF, from pre-procedure preparations to post-procedure care, is essential for those embarking on this path to parenthood.
Pre-Procedure Preparation:
Before diving into the IVF process, individuals or couples undergo thorough preparations. This typically begins with initial consultations with fertility specialists, where medical histories are reviewed, and personalized treatment plans are formulated. A series of fertility tests, including hormone evaluations and ovarian reserve assessments, may also be conducted to gauge fertility health accurately. These preparatory steps lay the foundation for a tailored IVF journey, ensuring that every aspect is meticulously planned to optimize the chances of success.
Ovarian Stimulation:
One of the pivotal stages in the IVF process is ovarian stimulation. This involves the administration of medications to stimulate the ovaries, encouraging the production of multiple eggs. The primary objective of ovarian stimulation is to increase the number of viable eggs available for retrieval during the subsequent phase. While this step is crucial for enhancing the success rates of IVF, it may also entail potential side effects such as bloating, mood swings, and ovarian hyperstimulation syndrome (OHSS). Close monitoring by fertility specialists helps mitigate risks and ensures optimal outcomes.
Monitoring:
Continuous monitoring of ovarian response is integral to the success of IVF. Through regular ultrasound scans and blood tests, fertility specialists track the growth and development of follicles within the ovaries. This real-time assessment allows for timely adjustments to medication dosages, ensuring that ovarian stimulation progresses optimally. The collaborative efforts between patients and medical professionals during this phase are instrumental in achieving the desired outcome of a successful IVF cycle.
Egg Retrieval:
The culmination of ovarian stimulation leads to the egg retrieval procedure, a minimally invasive technique guided by ultrasound. Under sedation or anesthesia, mature eggs are carefully aspirated from the ovaries using a fine needle. While discomfort during and after the procedure is minimal for most individuals, risks such as bleeding or infection are exceedingly rare. Egg retrieval marks a significant milestone in the IVF journey, bringing patients one step closer to realizing their dream of parenthood.
Sperm Collection and Preparation:
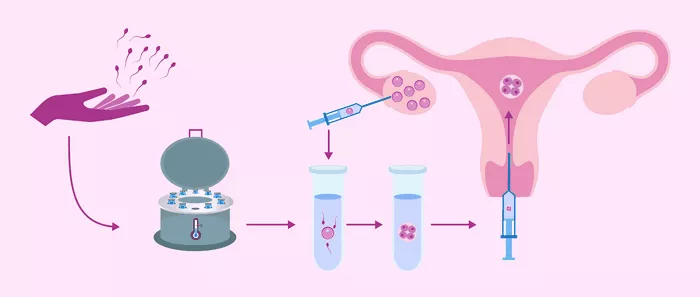
Simultaneous to egg retrieval, sperm samples undergo collection and preparation in the laboratory. Whether through ejaculation or surgical extraction techniques such as testicular sperm aspiration (TESA) or microsurgical epididymal sperm aspiration (MESA), the goal remains the same: to isolate healthy, motile sperm for fertilization. Sperm washing techniques are employed to remove seminal fluid and debris, ensuring optimal conditions for the fertilization process.
Fertilization:
In the controlled environment of the laboratory, the magic of fertilization unfolds as eggs and sperm are united through various techniques. Conventional IVF involves placing eggs and sperm together in a culture dish, allowing natural fertilization to occur. Alternatively, Intracytoplasmic Sperm Injection (ICSI) may be employed, where a single sperm is injected directly into an egg to facilitate fertilization. The choice between these methods depends on individual circumstances and recommendations from fertility experts.
Embryo Culture and Development:
Following fertilization, the resulting embryos are cultured and monitored closely as they undergo crucial developmental stages. Over several days, embryologists assess the quality and viability of embryos based on specific criteria, including cell division patterns and morphology. Selecting the healthiest embryos for transfer is paramount, maximizing the likelihood of successful implantation and pregnancy.
Embryo Transfer:
The eagerly anticipated embryo transfer procedure marks the culmination of the IVF cycle, as selected embryos are delicately transferred into the uterus. This minimally invasive procedure is performed under ultrasound guidance, using a thin catheter to deposit embryos at the optimal location within the uterine cavity. While the procedure itself is relatively brief and painless, patients may be advised to observe certain restrictions and recommendations in the aftermath to enhance the chances of implantation.
Post-Procedure Care and Follow-Up:
Following embryo transfer, patients are provided with comprehensive guidelines for post-procedure care. This typically includes a regimen of medications to support implantation and early embryo development, as well as recommendations for activity restrictions and lifestyle modifications. Scheduled follow-up appointments with the fertility clinic allow for ongoing monitoring and, ultimately, pregnancy testing to determine the success of the IVF cycle.
Success Rates and Potential Risks:
Understanding the factors influencing IVF success rates is crucial for managing expectations and making informed decisions. While age, underlying fertility issues, and previous treatment history play significant roles, advancements in technology and techniques have contributed to steadily improving success rates. Nonetheless, it’s essential to acknowledge the potential risks and complications associated with IVF, ranging from multiple gestations and ovarian hyperstimulation syndrome to rare instances of ectopic pregnancy or miscarriage.
Emotional Support:
Navigating the IVF journey can evoke a rollercoaster of emotions, from hope and anticipation to frustration and disappointment. Recognizing the emotional toll of infertility, many fertility clinics offer dedicated support services to assist patients and couples throughout the process. Whether through counseling, support groups, or online resources, seeking emotional support can provide invaluable comfort and guidance during challenging times.
Cost Considerations and Insurance Coverage:
While IVF offers a beacon of hope for those struggling with infertility, it’s essential to consider the financial implications associated with treatment. The cost of IVF varies widely depending on factors such as location, clinic reputation, and specific treatment protocols. While some insurance plans may offer partial coverage for fertility treatments, others may provide no coverage at all. Exploring alternative financing options or fertility grants can help alleviate the financial burden for individuals or couples pursuing IVF.
Alternative Options:
While IVF remains a cornerstone of assisted reproductive technology, it may not be the optimal choice for everyone. Fortunately, a range of alternative fertility treatments and procedures exists, catering to diverse needs and circumstances. From intrauterine insemination (IUI) and ovulation induction to third-party reproduction options such as egg donation or gestational surrogacy, individuals and couples are encouraged to explore alternative paths to parenthood with the guidance of fertility specialists.
Conclusion:
Embarking on the IVF journey is both a courageous decision and a profound leap of faith. As individuals and couples navigate the complexities of infertility treatment, they are met with unwavering support and expertise from dedicated fertility professionals. By understanding the various stages of the IVF process, from pre-procedure preparations to post-procedure care, patients can approach their journey with confidence and optimism. With perseverance, patience, and the support of their fertility community, dreams of parenthood can indeed become a reality.
Related Topics:
The TESA IVF Success Rates: What You Need to Know