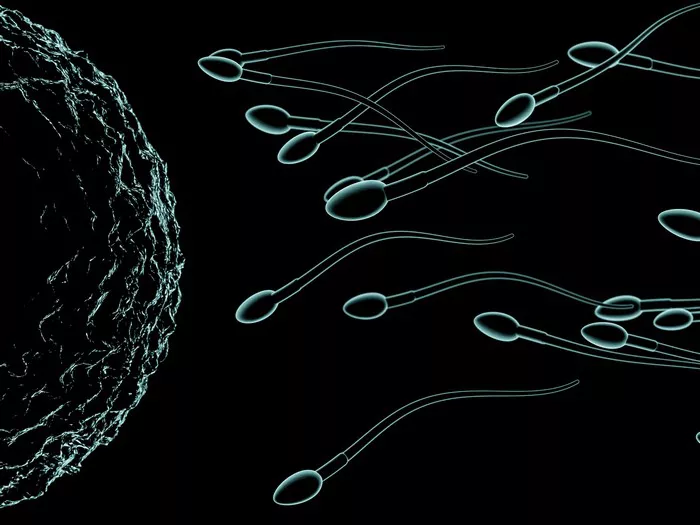
Retrograde ejaculation is a condition where semen, instead of being ejaculated out through the penis during orgasm, is redirected into the bladder. This occurs due to the failure of the bladder neck muscles to close properly during ejaculation. As a result, when a man with retrograde ejaculation reaches climax, little to no semen is expelled from the penis, giving the sensation of a dry orgasm. This condition differs from typical ejaculation, where semen is propelled outwards through the urethra.
Symptoms and Diagnosis:
Symptoms of retrograde ejaculation may include experiencing dry orgasms, cloudy urine after ejaculation due to semen being present in the bladder, and difficulty conceiving. The diagnostic process often involves a physical examination and a detailed medical history to identify any underlying conditions or factors contributing to retrograde ejaculation. Additionally, a post-ejaculatory urine sample may be analyzed to confirm the presence of semen in the bladder, indicative of retrograde ejaculation.
Causes:
There are several potential causes of retrograde ejaculation, including nerve damage resulting from conditions such as diabetes, spinal cord injury, or multiple sclerosis. Surgical procedures such as prostate surgery or bladder neck surgery can also disrupt the normal function of the muscles that control ejaculation, leading to retrograde ejaculation. Certain medications used to treat conditions like high blood pressure or depression may also have side effects that interfere with ejaculation.
Treatment Options:
Treatment options for retrograde ejaculation vary depending on the underlying cause and the severity of the condition. In cases where medication is the culprit, adjusting the dosage or switching to an alternative medication may alleviate symptoms. Alpha-adrenergic agonists, such as pseudoephedrine, can sometimes be prescribed to tighten the bladder neck muscles and prevent semen from entering the bladder during ejaculation. However, these medications may not be effective for everyone.
For individuals with severe retrograde ejaculation or those who do not respond to medication, surgical interventions may be considered. Surgical procedures, such as transurethral resection of the bladder neck or sperm retrieval techniques, aim to restore normal ejaculation function by correcting anatomical abnormalities or bypassing the issue altogether.
Lifestyle changes can also play a role in managing retrograde ejaculation. Avoiding alcohol and illicit drugs, which can exacerbate the condition, and practicing techniques to strengthen pelvic floor muscles may help improve ejaculatory function in some cases.
Impact on Fertility:
Retrograde ejaculation can significantly impact fertility since it reduces or eliminates the presence of semen in the ejaculate, making it difficult for couples to conceive through natural means. However, for individuals desiring parenthood, there are still options available. Techniques such as intrauterine insemination (IUI) or in vitro fertilization (IVF) can bypass the issue of retrograde ejaculation by retrieving sperm from the urine or directly from the testicles for use in assisted reproductive procedures.
Coping Strategies:
Dealing with retrograde ejaculation can be emotionally challenging for individuals and their partners. Open communication with healthcare providers and partners about concerns and feelings surrounding the condition is essential. Seeking support from a therapist or joining a support group for individuals with similar experiences can also provide valuable emotional support and coping strategies.
When to See a Doctor:
It is important to consult a healthcare professional if you experience symptoms of retrograde ejaculation, especially if you are concerned about fertility or overall sexual health. A doctor can perform a thorough evaluation to determine the underlying cause of the condition and recommend appropriate treatment options.
Success Rates and Prognosis:
The success rates of treatment for retrograde ejaculation vary depending on the cause and the chosen intervention. Medications may be effective for some individuals but not for others. Surgical procedures, while more invasive, can provide long-term relief for those with anatomical abnormalities contributing to retrograde ejaculation. Overall, with proper diagnosis and treatment, many individuals with retrograde ejaculation can achieve improved ejaculatory function and, in some cases, successful conception through assisted reproductive techniques.
Conclusion:
Retrograde ejaculation is a treatable condition that can have significant implications for fertility and sexual health. By understanding the causes, symptoms, and available treatment options, individuals affected by retrograde ejaculation can work with healthcare professionals to find effective solutions. While coping with the emotional and psychological aspects of this condition can be challenging, seeking support and guidance can help individuals and their partners navigate this journey towards improved sexual function and reproductive success. If you suspect you may have retrograde ejaculation, don’t hesitate to seek medical advice and explore the options available to you.